12-Lead ECG Placement Guide

Talk to my EMT partner about my biggest pet peeve, and aside from the lack of professionalism in the EMS industry, he’ll tell you I can’t stand people who do not know or practice proper 12-lead ECG placement. I’ve been in EMS for 5 years, and I’m sad to say I have never once seen someone apply a 12-lead properly. Don’t believe me? Just search “12-lead placement” in Google Images after reading this post and you’ll see that almost everyone is guilty.
What is an ECG?
An ECG stands for electrocardiogram. It is a tool used to detect a wide range of heart dysrhythmias using waveforms on a monitor. It is used by healthcare providers regularly both in the hospital and by EMS.
Why Is 12-Lead ECG Placement Important?
This is a big deal to me because I have on two occasions moved the someone else’s 12-lead ECG placement and identified a STEMI that was not visible with the original placement. On the flip side, recently I found a huge STEMI and when I got to the main heart hospital, the tech took my leads, moved them down, and couldn’t see the STEMI.
It’s terrible patient care! These patients sit in the ED for hours while they wait for their lab work to come back. Only then do they realize they’re having a heart attack. A lot of times this could be avoided if the 12-lead was performed properly and the STEMI was identified on the first go-around.
It takes literally less than 30 seconds to find the correct position for a 12-lead ECG placement! By the way, did you know that if your electrodes are off by 2 centimeters that it can completely skew your EKG morphology?
4-Lead Placement
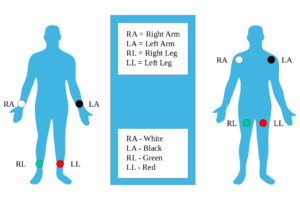
Before we can get to placing our precordial leads, we need to know where our 4-lead goes. Ever heard 4-leads referred to as “limb leads”? There’s a reason for that. These leads are not suppose to go anywhere on the torso. It’s not as big of a deal if you’re only doing a 4-lead, but doing so when you’re going to put the precordial leads on will alter the morphology of your EKG.
Limb leads can be placed on any part of the patient’s respective limbs. Just make sure the leads are symmetrical. For example, don’t put one lead on the left shoulder and the other lead on the right forearm. I’ve heard of one local doctor that preferred all 4 leads to be placed relatively equal distances distally. For example, if you put leads on the wrists, then leads should also go on the ankles. I haven’t found anything to back that, but that’s at least one professional’s theory.
The 12-lead ECG electrode placement is essential for paramedics and EMTs in both prehospital and hospital setting as incorrect placement can lead to false diagnosis of infarction or negatively change the EKG.
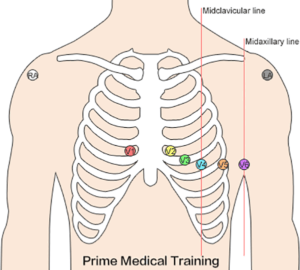
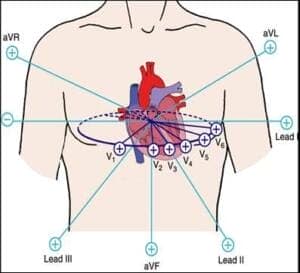
Proper 12-Lead ECG Placement
Now that we have our 4-leads straight, let’s talk about where your precordial leads will go. Everyone slaps them on below the breast and sometimes below the entire rib cage. That is completely unacceptable! Below is a bullet point list for each lead, a description of where they go, and the order they should be applied.
| ELECTRODE | PLACEMENT |
| V1 | 4th Intercostal space to the right of the sternum |
| V2 | 4th Intercostal space to the left of the sternum |
| V3 | Midway between V2 and V4 |
| V4 | 5th Intercostal space at the midclavicular line |
| V5 | Anterior axillary line at the same level as V4 |
| V6 | Midaxillary line at the same level as V4 and V5 |
| RL | Anywhere above the right ankle and below the torso |
| RA | Anywhere between the right shoulder and the wrist |
| LL | Anywhere above the left ankle and below the torso |
| LA | Anywhere between the left shoulder and the wrist |
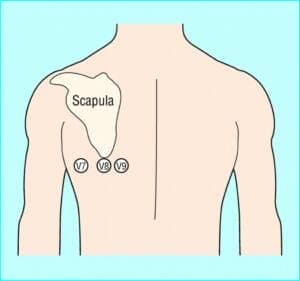
Aside from a 12-lead ECG placement, there’s something known as a 15-lead placement which includes placing leads V4-V6 on the posterior side of the patient below their left scapula (see below). When viewing the EKG strip, V4-V6 on the strip will be referred to as V-13-15. To clarify, leads will equal: V4=V7, V5=V8, and V6=V9.
Lastly, a right sided 12-lead ECG placement allows you to detect a right sided infarct. At a minimum, lead V4 should be placed on the 5th intercostal, mid-clavicular (exact opposite of the regular left side placement) if an inferior infarct was originally seen in leads II, III, and AVF.
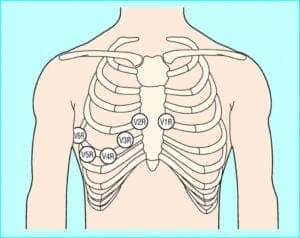
These give you more views of the heart and can help inform your treatment plans. For instance, you never want to give nitroglycerin if you see an inferior infarct until after performing a right-sided EKG. You can view these and other helpful diagrams.
Electrode Misplacement
- Up to 50 percent of cases have V1 and V2 in too high of a location which can mimic an anterior MI and cause T wave inversion. This article explains how to properly find the intercostal spaces and where to place the electrodes.
- Up to 33 percent of the cases have the precordial electrodes (V1-V6) lower or laterally misplaced which also leads to misdiagnosis.
12-Lead ECG Electrode Placement Explained
One of the most common questions related to 12-lead ECG electrode placement is why there are only 10 electrodes. It’s very important to understand what the term “lead” really means. A lead is a view of electrical activity of the heart from a specific angle across the body. So, even though you only have 10 leads, you are actually getting 12 views from different angles. Cables and Sensors does a great job explaining more of the morphology, vertical plane, and Einthoven’s Triangle.
Best Practices For 12-Lead ECG Electrode Placement
- Counting intercostals – When counting down to the 4th intercostal, it’s helpful to know that the 1st intercostal space is the space right below the clavicle.
- Clean surfaces – For our patients who seem adverse to hygiene, it’s important to clean the surface of dead tissue to get an accurate EKG reading. Taking a 4×4 of gauze and aggressively rubbing the area until it is pink will do the trick.
- The breast – Often times, the 5th intercostal space is about nipple line. On a guy, that’s ok, it doesn’t have have to be below the breast contrary to popular belief. Only for women with large breasts do we need to alter our placement and place the leads in the crest underneath the breast. This is because there is too much tissue to get a clear reading
- Look at trending – it’s recommended to get a baseline before giving oxygen or other medication and then performing multiple EKGs to see any how the patient is trending.
Reducing Artifact
The heart’s electrical signal has very little output, so it can easily be combined with other signals of identical frequency to create artifact. It is not uncommon to have some form of artifact for a 12-lead ECG placement but it’s important to attempt to lessen any interference in order to ensure an accurate EKG. The following are a few guidelines that are very helpful to reduce artifact while performing EKG’s.
- Place patient in a supine position if the patient will tolerate.
- Place the patient’s arms down by their side to relax their shoulders.
- Patient’s legs should be uncrossed.
- Electrical devices such as mobile phones should be away from the patient as these devices may interfere with the machine.
- Dry the skin if it is diaphoretic or moist.
- Shave any hair that can interfere with electrode placement.
- Electrode gel should be moist.
- Electrodes should not be placed over bones and over areas where there is a lot of muscle movement.
- Sometimes an abrasive material such as a wash cloth may need to be used to remove dead skin cells.
I hope this was a helpful review and that all of you will take it to “heart”. These are things we regularly go over in our ACLS and PALS classes. If you have comments or additions to what we covered, please let us know in the comments section below. If you’re looking for other great guides, check out what we wrote for using waveform capnography in cardiac arrest.
Vitali provides life-saving training taught by real emergency responders. You can view our current locations where we have regularly scheduled classes, or request for us to do on-site training at your location.


